How to interpret neuroassay results in autoimmune neurology is a critical skill for neurologists. Understanding antibody profiles, titers, and clinical context is essential for diagnosing and managing central nervous system (CNS) autoimmune disorders.

Understanding Autoantibody Profiles in CNS Autoimmunity
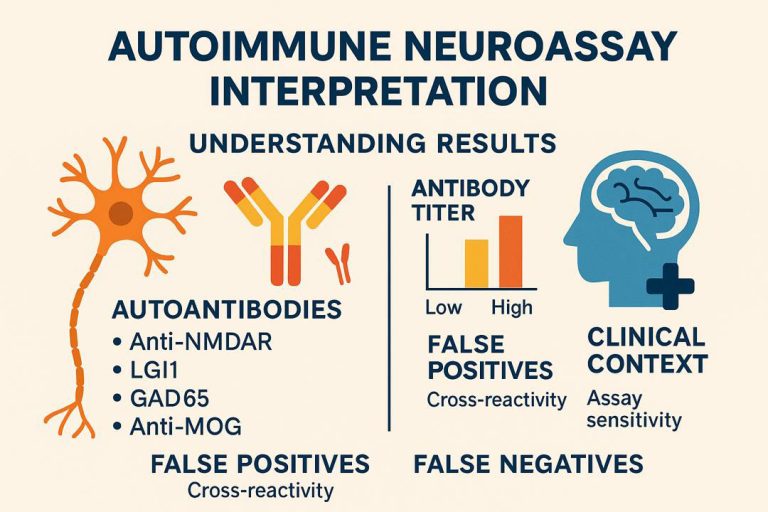
Autoimmune neurological diseases are characterized by specific antibodies targeting neuronal surface or intracellular antigens. Neuroassays help detect these antibodies in cerebrospinal fluid (CSF) or serum, offering diagnostic and prognostic value.
Key Autoantibodies in Autoimmune Neurology
- Anti-NMDA receptor (NMDAR)
- LGI1 and CASPR2 (limbic encephalitis)
- GAD65 (autoimmune epilepsy and stiff-person syndrome)
- Anti-MOG (demyelinating syndromes)
Interpreting Positive Results: Clinical Context Is Crucial
Neuroassay positivity must always be interpreted in light of clinical findings, imaging, and CSF analysis. A positive antibody result alone does not confirm autoimmune disease.
Consider These Key Factors:
- Antibody titer: Higher titers often correlate with active disease, but some antibodies (e.g., GAD65) may be present in low titers in non-pathological contexts.
- CSF vs. serum: CSF positivity is more specific, especially for NMDAR encephalitis. Some antibodies (e.g., LGI1) are usually detectable in serum.
- Symptom timing: Acute or subacute onset supports an autoimmune process.
Common Pitfalls in Neuroassay Interpretation
False Positives
Low-titer antibodies, cross-reactivity, and technical variability may lead to false positives, particularly when clinical correlation is poor.
False Negatives
Some antibodies may not be detected in serum, especially early in disease or if the assay is not optimized. CSF testing is often more sensitive.
When to Repeat Testing or Expand the Panel
If clinical suspicion is high but the initial panel is negative, repeat testing or using a broader panel (including cell-based assays) may be warranted. This is especially important in seronegative autoimmune encephalitis.
Case Example: Anti-NMDAR Encephalitis
A 22-year-old woman presents with psychiatric symptoms, seizures, and autonomic instability. CSF neuroassay reveals anti-NMDAR IgG antibodies. MRI is normal, but EEG shows diffuse slowing. Diagnosis of anti-NMDAR encephalitis is confirmed, guiding immunotherapy.
Clinical Integration and Decision-Making
Interpretation of neuroassays should support—not replace—clinical reasoning. Confirmatory tests, imaging, and therapeutic trials may all contribute to accurate diagnosis and patient care.
Guidelines and Further Reading
For updated guidance on autoimmune encephalitis, visit the Autoimmune Encephalitis Alliance, a trusted source for clinicians.